 *This is an article from the Fall 2023 issue of Contentment Magazine.
*This is an article from the Fall 2023 issue of Contentment Magazine.
By Brandon LaGreca, LAc, MAcOM
Does stress cause or promote cancer, and if so, can the stress response be influenced to prevent or help treat malignancy? To answer these questions requires a firm grasp of the science placed within the context of the many factors that contribute to cancer formation.
The basic framework of stress physiology elucidates the likely mechanisms of the stress-cancer connection. The earliest indication came from Hans Selye, MD documenting atrophy in the thymus gland in stressed rats. The elevation of glucocorticoids is widely accepted as the dominant mechanism for this effect. Stress also suppresses activity of T lymphocytes and natural killer cells, culminating in lowered immunity and increased tumor growth and development.1,2
Natural killer cells and T lymphocytes are two key players of cell-mediated immunity, the aspect of the immune system that patrols for and removes malignant cells. Of all the immune cell types, natural killer cells appear to be most significantly influenced by psychoneuroimmunology (PNI) factors. In addition, the PNI fallout from psychological stress is acknowledged to affect two additional aspects of carcinogenesis: DNA repair and regulation of apoptosis (programmed, healthy cell death that cancer cells circumnavigate).3 Although cancer formation falls squarely on exposure to carcinogens, a suppressed immune system allows precancerous cells to grow unchecked.

Biomedical research continues to explore the effect of stress on immunity. It was recently discovered that fragments of mitochondria (energy-generating organelles within the cytoplasm of cells) can be detected in the bloodstream following acute stress. This is called damage-associated molecular patterns, these mitochondrial fragments trigger immune and inflammatory pathways.4
This is particularly concerning considering mitochondrial dysfunction is being studied as a major player in oncogenesis. Elevated glucocorticoids from chronic stress also aid angiogenesis, the process by which cancer cells increase blood supply to rapidly fuel their metabolism with glucose. Paired with the fact that glucocorticoids raise blood sugar (often a cancer cell’s fuel of choice), these changes in the body’s terrain represent yet another mechanism of how stress promotes a cancer microenvironment.5
Pharmaceutical companies seek to leverage this aspect of tumor physiology by developing drug therapies targeting angiogenesis to slow the aggressiveness of certain cancers. Of course, a holistic approach to cancer treatment would not rely on therapies to blunt angiogenesis without acknowledging the lifestyle factors that promote angiogenesis. If a bathtub is overflowing, it is wise to first turn off the faucet before unclogging the drain.
Systemic inflammation also ensues from chronic stress. Elevated expression of the inflammatory cytokine interleukin-6 (IL-6) can be detected in epithelial tumors, implicating IL-6 with tumor formation and disease progression.6 The exact mechanism is unclear, and cytokine signaling can also have an antiapoptotic effect, yet elevated IL-6 can be observed in patients with different cancers and correlates with a poor prognosis. Whether these hallmarks of inflammation are the body’s healing response to cancer or oncology treatment, or an underlying risk factor to cancer development remains to be seen.
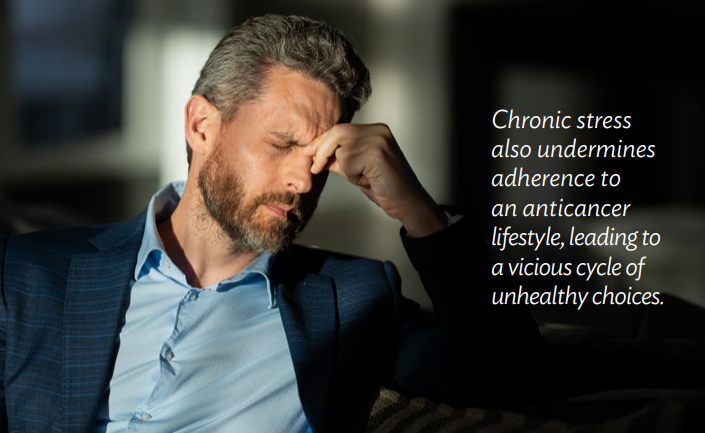
Chronic stress also undermines adherence to an anticancer lifestyle, leading to a vicious cycle of unhealthy choices. When daily work and home stress become a deterrent to proper self-care, sleep quality and quantity are often affected. Prolonged stress also leads to destructive behaviors that are carcinogenic, such as cigarette smoking to alleviate anxiety.

Then a health crisis — a cancer diagnosis — hits, compounding stress exponentially. Stress may not have been the textbook carcinogen in this case, but by insidiously feeding several cancer contributors, stress should be considered a root cause of cancer development. The effect is incremental and indirect, but powerful.
The effects of chronic stress and immune dysregulation are one line of evidence, but what about acute stress, activation of the sympathomedullary (SAM) pathway, and release of norepinephrine and epinephrine? Interestingly enough, pharmaceutical companies are well aware of this connection and are funding research to get beta-blocker drugs approved for cancer treatment and prevention based on their ability to antagonize norepinephrine and epinephrine receptors.7,8 
To these clear mechanisms suggesting that acute and chronic stress promote cancer progression can be added animal studies that show how controlled stress augments cancer formation. In one mouse model where tumors were induced by exposure to ionizing radiation, restraint stress was found to promote tumorigenesis through a loss of expression of a tumor-suppressor protein. Again, this effect is thought to be mediated by elevations in glucocorticoids (cortisol).9
Animal models also report several related mechanisms of cancer progression from stress, including increased angiogenesis via enhanced expression of growth factors.10
The case for cancer initiation in animal studies is less clear but suggestive of the ability of stressful conditions to jump-start latent malignancy that might not have manifested due to healthy immune surveillance. A number of stresses, including a breakdown in social order, create an immunocompetence sufficient to significantly increase tumor formation in mice when compared to unstressed controls.11,12

Epidemiological Evidence
Mice in lab experiments is one thing, but what about cancer initiation in humans from acute and chronic stress? A few lines of evidence suggest that elevated stress hormones can directly damage DNA and protect cancer cells from apoptosis (programmed cell death), a double whammy for tumorigenesis.13,14
A model of all these collective mechanisms — immune and metabolic dysregulation, inflammation, altered expression of tumor-suppressor proteins, DNA damage — opens the door for translation research to posit that stress may indeed underlie cancer formation.15
Of course, stress is only one of many carcinogens that people may be exposed to. Yet the weight of evidence clearly places stress as a significant promoter of cancer progression and influencer of cancer relapse, chemoresistance, angiogenesis, and metastasis.16,17,18
Biochemistry aside, a broader brushstroke reveals that psychosocial factors also influence cancer incidence and progression. Although the mechanism resides in the field of PNI, the precipitating cause may stem from big-picture psychosocial factors such as disruptions in a healthy diet, sleep, and exercise.19,20
In the same vein, depression and a lack of social support have been identified as risk factors for the development of cancer.21,22
Epidemiological studies in humans support this notion, with feelings of helplessness being associated with 160% more fatal cancers, losing an emotional relationship doubling the risk of breast cancer, and feeling alone when dealing with a trauma resulting in a 9 times greater risk of developing breast cancer.23,24,25
Research Controversy
The evidence detailed here may not persuade a skeptic that stress should be classified as a textbook carcinogen. “Stress causes cancer” is a bold claim.
Stress unequivocally affects cancer progression in animal studies, but that is a difficult conclusion to scale to humans. For one, we’re a different species. Perhaps humans have evolved with better capacities to handle stress; the human higher brain affords some interesting stress-interrupting possibilities.
Another factor is that animal studies rely on tumors being artificially induced, typically from a single carcinogen or mutagenic virus. This is completely out of context with the environment in which human tumors develop, replete with multiple carcinogenic influences and cancer-promoting lifestyle factors.26
Most human studies are retrospective, looking back and attempting to correlate ongoing stress or a major trauma with cancer incidence. This level of evidence is vulnerable to confirmation bias and the shifting sands of human memory. The concern is that the reporting patient is more likely to associate stress with cancer development than someone who has not received such a devastating diagnosis.
Stress perception also plays a role. There is an inkling in the research literature that being stressed poses one risk and feeling stressed an additional one. The difference may seem subtle, but the perception that stress is damaging one’s health adds yet another layer to the problem, and humans are uniquely capable of feeling this. The catastrophizing human brain can elicit a stress response worse than what the stress stimulus itself would otherwise cause.27
Taken collectively, animal studies, mechanistic research, and epidemiological surveys of psychosocial factors provide a framework for understanding the stress-cancer connection. How potent that influence is will be determined in time with further research into stress physiology and strategies to negate the negative effects of chronic stress.28
Science is a waiting game, but given the evidence presented here, it is up to the individual to determine how impactful stress is in their life and, if diagnosed with cancer, the degree that stress underlies the disease process you are positioning yourself to overcome.
Disclosure Statement: Portions of this article have been excerpted from Brandon’s book, Cancer, Stress & Mindset: Focusing the Mind to Empower Healing and Resilience, available on his website BrandonLaGreca.com and through online retailers.
References
- Anisman H., Irwin J., Sklar L.S. (1989) “The Influence of Stressors on the Progression of Neoplastic Change.” In: Weisburger E.K. (eds) Mechanisms of Carcinogenesis. Cancer Growth and Progression, vol 2. Springer, Dordrecht. https://doi.org/10.1007/978-94-009-2526-7_2.
- Mavoungou, E., M. K. Bouyou-Akotet, and P. G. Kremsner. “Effects of Prolactin and Cortisol on Natural Killer (NK) Cell Surface Expression and Function of Human Natural Cytotoxicity Receptors (NKp46, NKp44 and NKp30).” Clinical & Experimental Immunology 139, no. 2 (February 1, 2005): 287–96. https://doi.org/10.1111/j.1365-2249.2004.02686.x.
- Kiecolt-Glaser, J. K., T. F. Robles, K. L. Heffner, T. J. Loving, and R. Glaser. “Psycho-Oncology and Cancer: Psychoneuroimmunology and Cancer.” Annals of Oncology 13, no. suppl_4 (October 1, 2002): 165–69. https://doi.org/10.1093/annonc/mdf655.
- Sheikh, Knvul. “Brain’s Dumped DNA May Lead to Stress, Depression.” Scientific American. https://www.scientificamerican.com/article/brain-rsquo-s-dumped-dna-may-lead-to-stress-depression/. (accessed 15 November 2019).
- Winters, Nasha, and Jess Higgins Kelley. The Metabolic Approach to Cancer: Integrating Deep Nutrition, the Ketogenic Diet, and Nontoxic Bio-Individualized Therapies. Chelsea Green Publishing, 2017.
- Schafer, Zachary T., and Joan S. Brugge. “IL-6 Involvement in Epithelial Cancers.” The Journal of Clinical Investigation 117, no. 12 (December 3, 2007): 3660–63. https://doi.org/10.1172/JCI34237.
- Fitzgerald, Paul J. “Beta Blockers, Norepinephrine, and Cancer: An Epidemiological Viewpoint.” Clinical Epidemiology 4 (2012): 151–56. https://doi.org/10.2147/CLEP.S33695.
- Powe, Desmond G., Melanie J. Voss, Kurt S. Zänker, Hany O. Habashy, Andrew R. Green, Ian O. Ellis, and Frank Entschladen. “Beta-Blocker Drug Therapy Reduces Secondary Cancer Formation in Breast Cancer and Improves Cancer Specific Survival.” Oncotarget 1, no. 7 (November 2010): 628–38. https://doi.org/10.18632/oncotarget.197.
- Feng, Zhaohui, Lianxin Liu, Cen Zhang, Tongsen Zheng, Jiabei Wang, Meihua Lin, Yuhan Zhao, Xiaowen Wang, Arnold J. Levine, and Wenwei Hu. “Chronic Restraint Stress Attenuates P53 Function and Promotes Tumorigenesis.” Proceedings of the National Academy of Sciences, April 12, 2012, 201203930. https://doi.org/10.1073/pnas.1203930109.
- Thaker, Premal H., Susan K. Lutgendorf, and Anil K. Sood. “The Neuroendocrine Impact of Chronic Stress on Cancer.” Cell Cycle 6, no. 4 (February 15, 2007): 430–33. https://doi.org/10.4161/cc.6.4.3829.
- Riley, V. “Psychoneuroendocrine Influences on Immunocompetence and Neoplasia.” Science 212, no. 4499 (June 5, 1981): 1100. https://doi.org/10.1126/science.7233204.
- Henry, James P., Patricia M. Stephens, and Flora M. Watson. “Force Breeding, Social Disorder and Mammary Tumor Formation in CBA/USC Mouse Colonies: A Pilot Study.” Psychosomatic Medicine 37, no. 3 (June 1975): 277–83. https://doi.org/10.1097/00006842-197505000-00006.
- Flint, Melanie S., Andrew Baum, William H. Chambers, and Frank J. Jenkins. “Induction of DNA Damage, Alteration of DNA Repair and Transcriptional Activation by Stress Hormones.” Psychoneuroendocrinology 32, no. 5 (June 1, 2007): 470–79. https://doi.org/10.1016/j.psyneuen.2007.02.013.
- Sastry, Konduru S. R., Yelena Karpova, Sergey Prokopovich, Adrienne J. Smith, Brian Essau, Avynash Gersappe, Jonathan P. Carson, et al. “Epinephrine Protects Cancer Cells from Apoptosis via Activation of CAMP-Dependent Protein Kinase and BAD Phosphorylation.” The Journal of Biological Chemistry 282, no. 19 (May 2007): 14094–100. https://doi.org/10.1074/jbc.m611370200.
- Jenkins, Frank J., Bennett Van Houten, and Dana H. Bovbjerg. “Effects on DNA Damage and/or Repair Processes as Biological Mechanisms Linking Psychological Stress to Cancer Risk.” Journal of Applied Biobehavioral Research 19, no. 1 (March 1, 2014): 3–23. https://doi.org/10.1111/jabr.12019.
- Nagaraja, Archana S., Guillermo N. Armaiz-Pena, Susan K. Lutgendorf, and Anil K. Sood. “Why Stress Is BAD for Cancer Patients.” The Journal of Clinical Investigation 123, no. 2 (February 1, 2013): 558–60. https://doi.org/10.1172/JCI67887.
- Armaiz-Pena, Guillermo N., Susan K. Lutgendorf, Steve W. Cole, and Anil K. Sood. “Neuroendocrine Modulation of Cancer Progression.” Brain, Behavior, and Immunity 23, no. 1 (January 1, 2009): 10–15. https://doi.org/10.1016/j.bbi.2008.06.007.
- Moreno-Smith, Myrthala, Susan K. Lutgendorf, and Anil K. Sood. “Impact of Stress on Cancer Metastasis.” Future Oncology 6, no. 12 (December 1, 2010): 1863–81. https://doi.org/10.2217/fon.10.142.
- Spiegel, David, and Pamela M. Kato. “Psychosocial Influences on Cancer Incidence and Progression.” Harvard Review of Psychiatry 4, no. 1 (January 1, 1996): 10–26. https://doi.org/10.3109/10673229609030518.
- Forlenza, Michael J., and Andrew Baum. “Psychosocial Influences on Cancer Progression: Alternative Cellular and Molecular Mechanisms.” Current Opinion in Psychiatry 13, no. 6 (2000). https://journals.lww.com/co-psychiatry/Fulltext/2000/11000/Psychosocial_influences_on_cancer_progression_.29.aspx.
- Reiche, Edna Maria Vissoci, Sandra Odebrecht Vargas Nunes, and Helena Kaminami Morimoto. “Stress, Depression, the Immune System, and Cancer.” The Lancet Oncology 5, no. 10 (October 1, 2004): 617–25. https://doi.org/10.1016/S1470-2045(04)01597-9.
- Antoni, Michael H., Susan K. Lutgendorf, Steven W. Cole, Firdaus S. Dhabhar, Sandra E. Sephton, Paige Green McDonald, Michael Stefanek, and Anil K. Sood. “The Influence of Bio-Behavioural Factors on Tumour Biology: Pathways and Mechanisms.” Nature Reviews Cancer 6, no. 3 (March 1, 2006): 240–48. https://doi.org/10.1038/nrc1820.
- Lillberg, Kirsi, Pia K. Verkasalo, Jaakko Kaprio, Lyly Teppo, Hans Helenius, and Markku Koskenvuo. “Stressful Life Events and Risk of Breast Cancer in 10,808 Women: A Cohort Study.” American Journal of Epidemiology 157, no. 5 (March 1, 2003): 415–23. https://doi.org/10.1093/aje/kwg002.
- Chida, Yoichi, Mark Hamer, Jane Wardle, and Andrew Steptoe. “Do Stress-Related Psychosocial Factors Contribute to Cancer Incidence and Survival?” Nature Clinical Practice Oncology 5, no. 8 (August 1, 2008): 466–75. https://doi.org/10.1038/ncponc1134.
- Price, Melanie A., Christopher C. Tennant, Phyllis N. Butow, Ross C. Smith, Susan J. Kennedy, Marjorie B. Kossoff, and Stewart M. Dunn. “The Role of Psychosocial Factors in the Development of Breast Carcinoma: Part II.” Cancer 91, no. 4 (February 15, 2001): 686–97. https://doi.org/10.1002/1097-0142(20010215)91:4<686::AID-CNCR1052>3.0.CO;2-0.
- Fitzmaurice, Mary Anne. “Physiological Relationships Among Stress, Viruses, and Cancer in Experimental Animals.” International Journal of Neuroscience 39, no. 3–4 (January 1, 1988): 307–24. https://doi.org/10.3109/00207458808985718.
- Keller, Abiola, Kristin Litzelman, Lauren E. Wisk, Torsheika Maddox, Erika Rose Cheng, Paul D. Creswell, and Whitney P. Witt. “Does the Perception That Stress Affects Health Matter? The Association with Health and Mortality.” Health Psychology 31, no. 5 (2012): 677. https://doi.org/10.1037/a0026743.
- Zhang, Z., Wang Y., and Li, Q. “Mechanisms Underlying the Effects of Stress on Tumorigenesis and Metastasis.” International Journal of Oncology 53, no. 6 (2018): 2332. https://doi.org/10.3892/ijo.2018.4570.