Measuring the Stress Response
By Brandon LaGreca, LAc, MAcOM
*This is an article from the Spring 2023 issue of Combat Stress
For military personnel and first responders, performing under stressful conditions comes as part of the job. Quantifying how stress affects the individual is an evolving science. This article explores the history of assessments that evaluate the health of the vagus nerve, part of the parasympathetic nervous system, or measure the release of stress hormones. To best understand one’s resilience to stressful situations, it is important to document these effects with proven metrics.
Before lab testing, holistic healthcare providers assessed stress resilience in a number of clever ways, several of which were centered on the health and function of the adrenal glands. One example is Ragland’s test. This involves taking a patient’s blood pressure after several minutes, while the patient lies in a relaxed state, followed by a second measurement taken as the patient rises to stand. The sudden change of position and consequent need to quickly get blood to the head is thought to be influenced by adrenal hormones. Lightheadedness upon rising (orthostatic hypotension) was considered a sign of adrenal insufficiency.
A method taught within naturopathic medicine to assess vagal tone, and by extension the resilience of the parasympathetic nervous system, is the evaluation of palatal rise. The levator veli palatini muscle, responsible for the rising and falling of the oral palate, is directly innervated by the vagus nerve. Having a patient stick out the tongue and say “aah” (more often used to check the health of the tonsils) is a window to observe the evenness of how the palate appears and how quickly it moves. Asymmetry and sluggish rising of the palate is considered a sign of poor vagal tone.
How precise these tests are at addressing autonomic nervous system health is debatable. Such methods formed the backbone of manual evaluation by old-school practitioners, who either didn’t have access to laboratory assessment or were practicing before the chemical analysis of hormone health was available.
Early 1960s research in psychophysiology relied on several methods of quantifying the stress response, including measuring changes in heart rate, respiration, and electrodermal response (such as with polygraph machines to gauge the subtle stress markers that may indicate that a person is lying).1
By the 1970s, heart rate variability (HRV) entered the scene, offering a new level of sophistication by measuring the minute but healthy change (variability) in the interval between each heartbeat as a marker of stress resilience and optimal vagal tone.2
With significant refinement to the technology over the last few decades, HRV has become the dominant player in the emerging science of biofeedback, allowing the user to precisely track the stress and relaxation response in real time. The health of the parasympathetic nervous system can be read like an open book in the heart’s variability, with HRV acting as an explicit indicator of vagal tone. The HeartMath Institute is on the forefront of HRV testing, churning out research and scaling HRV-measuring technology so that precise and affordable devices are now available to consumers.3 
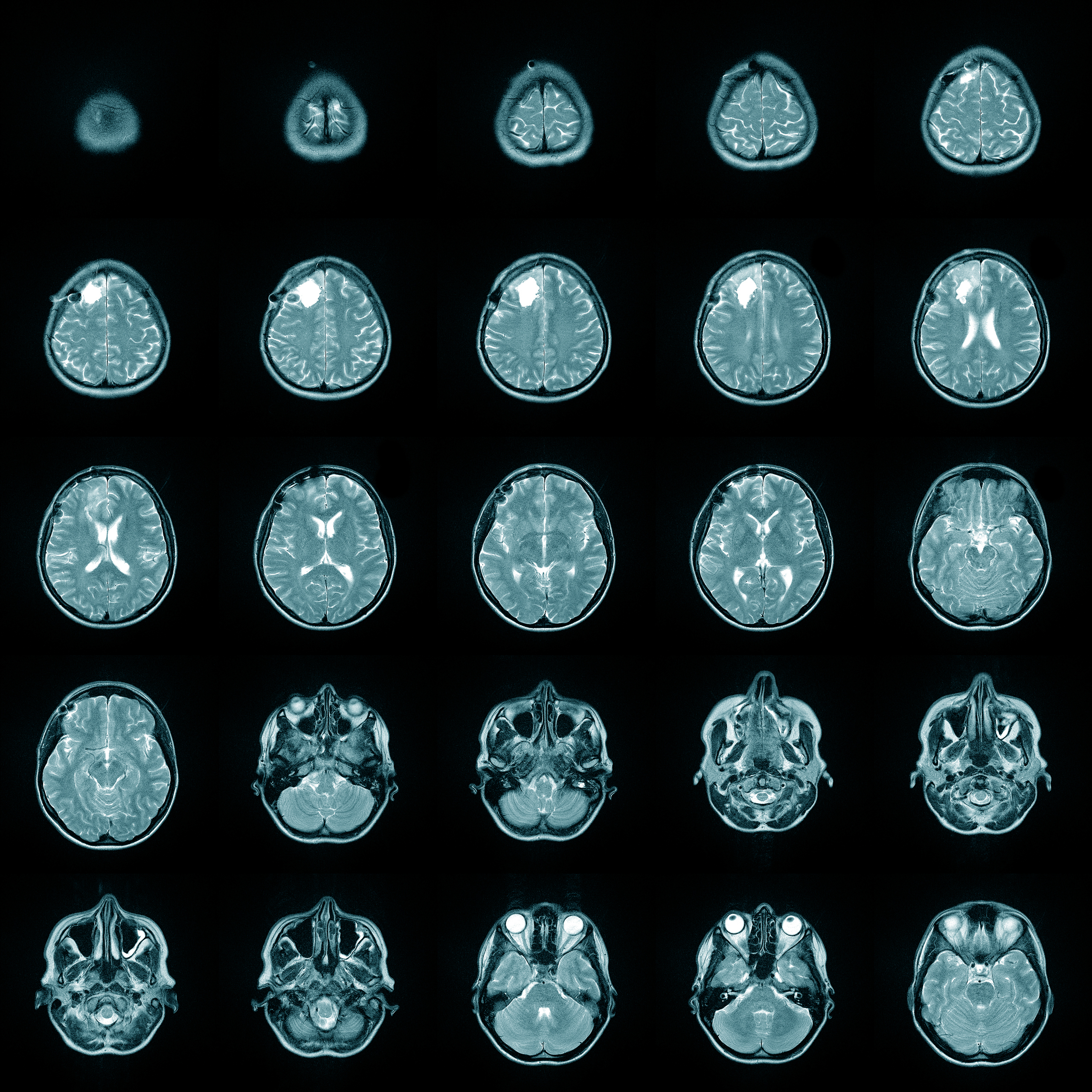
In an outpatient setting, conventional medicine favors brain imaging through functional MRI (fMRI) or single-photon emission computed tomography (SPECT) scans to visualize central nervous system health, while bloodwork is the standard for determining hormone levels. These methods are well-validated for diagnosis, but they have flaws. One problem with using bloodwork to assess hormone levels is that hormones travel bound to proteins when circulating in the bloodstream. Only by extrapolation can active levels of hormone levels be assessed, if at all.
To measure active or free levels of cortisol, sampling saliva is a method preferred by holistic healthcare providers. When I began private practice, I ordered cortisol panels that required the patient to collect a saliva sample (spit in a tube) four times a day to graph the rhythm of cortisol release. Cortisol is highest in the morning, peaks shortly after rising, slopes downward through the day, and is lowest at night as melatonin rises and the body prepares for slumber.
In those early days of cortisol testing, a four-point saliva panel was a game changer. Testing a patient with a diagnosis of chronic fatigue often revealed a flatlined cortisol rhythm, with a total cortisol level below average. This led to the then-vogue diagnosis of adrenal insufficiency (or adrenal fatigue).
Another common pattern observed is an inversion, whereby cortisol is low in the morning and spikes in the evening. This illustrates the classic “wired-and-tired” patient who experiences nonrestorative sleep—waking tired and needing stimulants (caffeine) to get going in the morning, only to find themselves “jacked up” and unable to wind down at the end of the day (evidenced by the evening spike in cortisol).
These assessments were convenient and directed successful clinical interventions, but they were not the most precise in terms of what is happening at the level of cellular human physiology. The true clinical picture became clear with the inclusion of urine testing to measure metabolized levels of hormones such as cortisol, estrogen, and progesterone. Introduced by the lab Precision Analytical, the dried urine test for comprehensive hormones, or DUTCH test, utilizes four urine samples taken throughout the day to derive a daily cortisol rhythm while sussing out the amount of metabolized hormones that pass through the kidneys to be excreted.
Measuring cortisone (cortisol deactivated in the colon, kidneys, and salivary glands) in addition to cortisol led to an important clinical discovery. Some patients previously diagnosed as having adrenal insufficiency turned out to be excreting high levels of cortisol metabolites. It wasn’t an issue of a lack of cortisol, rather, there was a lack of communication between the brain and glands to properly regulate hormone levels. This led to the more precise diagnosis of HPA-axis dysfunction, denoting the disharmony inherent from chronically elevated levels of cortisol that downregulate signaling hormones in the brain.
These patients were producing adrenal hormones, sometimes excessively, but the net effect on the body was a decreased action of those hormones at the appropriate sites. This is analogous to the vigorous production of insulin, yet lack of cellular response to shuttle sugar into the cells in patients with type 2 diabetes.
Metabolized hormone levels are an important piece of the puzzle, but because saliva was still relevant to assess adrenal resilience, Precision Analytical added another metric, using four saliva samples to derive what is known as cortisol awakening response (CAR).
Measuring CAR involves taking three saliva samples within the first 60 minutes of rising to see how vigorously and appropriately cortisol surges and how that effect is maintained during the initial timeframe of waking. Research suggests testing CAR is a clinically relevant assessment of adrenal health.4,5
The rhythm of cortisol release is predictive of stress resilience. The door swings the other way too, with a dysregulated cortisol rhythm suggestive of disease. One study indicated an abnormal or flattened cortisol rhythm is predictive of early mortality from breast cancer.6 
Testing cortisol can also serve as a proxy to assess potential environmental stressors. One paper showed how prolonged exposure to fluorescent lamps appreciably lowered cortisol levels. Readers of my first book, Cancer and EMF Radiation: How to Protect Yourself from the Silent Carcinogen of Electropollution, will not be surprised by this revelation, given the detrimental electromagnetic field emitted by fluorescent lights.7
The reverse has been studied. Early morning bright light exposure raises cortisol to healthy levels, while alterations to circadian rhythm through shift work or daylight-saving time affect optimal cortisol output.8,9
An important point to make at this juncture is that testing guides treatment in the context of a patient’s overall health. There is no one-size-fits-all approach, and wise holistic healthcare providers are cautious to pursue treatments that tweak hormones based on lab results alone.
Hormesis reigns supreme with hormone balance. Too much cortisol is as problematic as too little. Elevated norepinephrine is key to survival when the sympathetic nervous system is activated, but chronically high levels can lead to hormonal chaos.
It is possible to “bio-hack” these hormones with chemical therapies, from amino acids to prescription drugs. Beta blockers will blunt the effects of elevated norepinephrine at the cost of side effects inherent from altering normal human biochemistry.10 For cortisol, phosphatidylserine lowers elevated levels and hydrocortisone replaces and suppresses output.11
These substances all have their place and can be important tools, provided that dependency does not ensue from their use. This is especially true of hydrocortisone, as doses above physiological limits released by the adrenal glands cause a profound downregulation of the body’s ability to produce cortisol. For this reason, high doses of steroid drugs are prescribed with a gradual tapering of dosage over several days (if not weeks). Failure to do so may lead to the iatrogenic version of Addison’s disease when the adrenal glands fail to rebound following pharmaceutical suppression.
Herbal medicine offers a wise approach to managing hormone imbalances, not because nature’s pharmacy is inherently safe (though often it is), but because many herbs that address hormone problems are normalizing, meaning they can signal the brain to either raise or lower hormone levels depending on need. These responses occur within the body’s design and don’t force biochemical reactions like a drug does. To learn more about the safe use of adaptogenic herbs, consult a licensed healthcare provider educated in functional or integrative medicine.
Portions of this article have been excerpted from Brandon’s book, Cancer, Stress & Mindset: Focusing the Mind to Empower Healing and Resilience, available on his website BrandonLaGreca.com and through online retailers.
References
1. Stern, John A. “Toward a Definition of Psychophysiology.” Psychophysiology 1, no. 1 (1964): 90–91. https://doi.org/10.1111/j.1469-8986.1964.tb02626.x.
2. Berntson, Gary G., J. Thomas Bigger, Dwain L. Eckberg, Paul Grossman, Peter G. Kaufmann, Marek Malik, Haikady N. Nagaraja, et al. “Heart Rate Variability: Origins, Methods, and Interpretive Caveats.” Psychophysiology 34, no. 6 (1997): 623–48. https://doi.org/10.1111/j.1469-8986.1997.tb02140.x.
3. McCraty, Rollin, Bob Barrios-Choplin, Deborah Rozman, Mike Atkinson, and Alan D. Watkins. “The Impact of a New Emotional Self-Management Program on Stress, Emotions, Heart Rate Variability, DHEA and Cortisol.” Integrative Physiological and Behavioral Science 33, no. 2 (April 1, 1998): 151–70. https://doi.org/10.1007/BF02688660.
4. Clow, Angela, Frank Hucklebridge, Tobias Stalder, Phil Evans, and Lisa Thorn. “The Cortisol Awakening Response: More than a Measure of HPA Axis Function.” Neuroscience & Biobehavioral Reviews, Psychophysiological Biomarkers of Health, 35, no. 1 (September 1, 2010): 97–103. https://doi.org/10.1016/j.neubiorev.2009.12.011.
5. Fries, Eva, Lucia Dettenborn, and Clemens Kirschbaum. “The Cortisol Awakening Response (CAR): Facts and Future Directions.” International Journal of Psychophysiology, 72, no. 1 (April 1, 2009): 67–73. https://doi.org/10.1016/j.ijpsycho.2008.03.014.
6. Sephton, Sandra E., Robert M. Sapolsky, Helena C. Kraemer, and David Spiegel. “Diurnal Cortisol Rhythm as a Predictor of Breast Cancer Survival.” JNCI: Journal of the National Cancer Institute 92, no. 12 (June 21, 2000): 994–1000. https://doi.org/10.1093/jnci/92.12.994.
7. Jung, Christopher M., Sat Bir S. Khalsa, Frank A. J. L. Scheer, Christian Cajochen, Steven W. Lockley, Charles A. Czeisler, and Kenneth P. Wright. “Acute Effects of Bright Light Exposure on Cortisol Levels.” Journal of Biological Rhythms 25, no. 3 (May 19, 2010): 208–16. https://doi.org/10.1177/0748730410368413.
8. Hadlow, Narelle C., Suzanne Brown, Robert Wardrop, and David Henley. “The Effects of Season, Daylight Saving and Time of Sunrise on Serum Cortisol in a Large Population.” Chronobiology International 31, no. 2 (March 1, 2014): 243–51. https://doi.org/10.3109/07420528.2013.844162.
9. Thorn, L., F. Hucklebridge, A. Esgate, P. Evans, and A. Clow. “The Effect of Dawn Simulation on the Cortisol Response to Awakening in Healthy Participants.” Psychoneuroendocrinology 29, no. 7 (August 1, 2004): 925–30. https://doi.org/10.1016/j.psyneuen.2003.08.005.
10. Fitzgerald, Paul J. “Beta Blockers, Norepinephrine, and Cancer: An Epidemiological Viewpoint.” Clinical Epidemiology 4 (2012): 151–56. https://doi.org/10.2147/CLEP.S33695.
11. Benton, D., R.T. Donohoe, B. Sillance, and S. Nabb. “The Influence of Phosphatidylserine Supplementation on Mood and Heart Rate When Faced with an Acute Stressor.” Nutritional Neuroscience 4, no. 3 (January 1, 2001): 169–78. https://doi.org/10.1080/1028415X.2001.11747360.